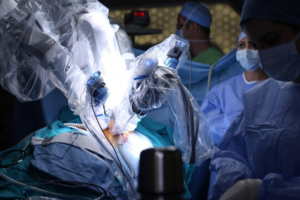
Robotic Hernia Surgery is a fast-evolving surgical technique. During robotic hernia repair, your surgeon is seated at a console next to you, operating through small surgical cuts utilizing miniature surgical tools and a 3D high-definition camera.
Afterward, patients typically experience pain and soreness from hernia repair surgery. However, this can be managed with over-the-counter pain medications.
Robotic Hernia Surgery is less invasive than other types of surgery for hernias. Instead of one large incision in the abdomen, small incisions are used. This helps reduce the risk of complications after the surgery, including pain and scarring. The procedure also allows patients to return to their normal routines more quickly than if they underwent traditional open surgery.
The robotic system enables surgeons to perform delicate operations with greater precision. It also provides more visualization of the surgical site. This helps your surgeon to more accurately repair hernias, so that your hernia doesn’t recur. While robotic hernia surgery is safe for most people, it’s important to discuss the risks with your doctor before you decide to undergo this treatment.
In the robotic-assisted hernia procedure, your surgeon sits at a console and uses master controls that function like forceps to maneuver miniaturized endoscopic instruments into the surgical site. The console then translates your surgeon’s commands into precise movements of the robotic arms. These movements enable your surgeon to stitch the muscle wall and prevent a hernia from protruding through this weak area of the stomach wall.
During a robotic inguinal hernia repair, your surgeon creates three ports: a 12 mm port near the belly button and two 8 mm ports on each side of the abdominal wall. This allows the surgeon to view the hernia from different angles and easily dissect the tissue surrounding it. Once the hernia is removed, the abdominal wall is reinforced with a mesh for strength support. The mesh is placed in the extraperitoneal space, so it doesn’t come into contact with the intestines.
Similarly, robotic ventral hernia repair uses the same approach to access the pre-peritoneal space, with the exception that we dissect Cooper’s ligament before relocating the peritoneal flap. This helps to identify the type of hernia (direct or indirect) and allows us to place the mesh appropriately without the potential for hernia recurrence.
In general, robotic hernia surgeries use fewer incisions, less cutting of muscles, and fewer stitches, so patients have fewer noticeable scars after the procedure. This also means that patients experience less pain after hernia surgery. This can help them recover more quickly so they can return to their normal activities sooner and feel healthier, more confident, and stronger after the surgery.
Minimally Invasive
Using surgical robots to perform hernia surgery reduces the amount of damage to the abdominal wall muscles and tissues and is associated with lower risks, quicker recovery and less pain. During a hernia repair procedure, the surgeon makes a series of small incisions to access the abdomen and insert specialized robotic instruments to remove the tissue protruding through the hernia and place a mesh patch to prevent it from occurring again. The surgeon may use the robotic tools to perform complex abdominal wall reconstruction techniques, which require a lot of sewing and dissection. These techniques would be difficult or impossible to perform with standard laparoscopy due to the size and complexity of the abdomen and hernia repair.
Michigan Hernia Surgery performs hernia surgery using the daVinci robot, which has three distinct parts. The first is the “brain” of the robot, which houses the camera, power and energy. The surgeon sits at a console next to the patient and controls the robot’s arms with hand-held controllers.
The surgeon’s movements are replicated by the robot, allowing the surgeon to perform surgery with increased precision and accuracy. The daVinci robot is used by surgeons in other specialties, including urology and gynecology, because of the benefits it offers, which include smaller incisions, faster recovery and decreased risk of complications.
In experienced hands, robotic hernia surgery can be safer than traditional open surgery and laparoscopic hernia repair. Patients are discharged from the hospital earlier, experience less pain and need fewer narcotic pain medications than with traditional hernia surgery. They can also return to work more quickly.
While robotic hernia surgery is a viable option for many patients, it is not the right solution for every person with a hernia. The type of hernia, other medical conditions and previous surgeries are all factors in deciding which surgical technique will be the best for you.
The daVinci robot is a cutting-edge technology that can be used for delicate and complex surgeries of the chest and abdomen, including hernias. It is also used to perform Heller myotomy, a procedure for achalasia, a condition where the lower esophageal sphincter does not relax properly, making it difficult to swallow food and liquids.
Precise
Using a robotic console that mirrors the surgeon’s hand and arm movements, every move your doctor makes on the console is translated into bending and rotating instruments within the hernia site. This enables your doctor to access and repair the hernia through small incisions. It also helps minimize tissue damage and pain.
Surgeons are able to see blood vessels and other structures with the high-definition camera on the surgical console, allowing them to work more precisely. This has led to significantly fewer complications during surgery and better hernia repairs compared to traditional open surgery. It has also helped reduce post-surgical pain, enabling patients to take less pain medication and recover faster.
While robot-assisted hernia surgery is an excellent option for many patients, it is not right for everyone. Whether it is due to other medical conditions, previous surgeries or hernia size and location, not all hernias can be safely repaired with robot-assisted techniques. If your hernia is not suitable for robotic hernia surgery, your doctor will explain your options and recommend the most appropriate treatment.
In robotic hernia surgery, your surgeon sits at a console next to you and operates through small incisions on the abdomen. They then view a magnified, high-definition 3D image inside your body to guide them through the procedure. They introduce miniaturized instruments through a few tiny incisions and use master controls that function like forceps.
Because of the stability and magnification on the console, surgeons feel more comfortable during robotic hernia surgery. Moreover, the surgical tools are much easier to handle – especially in tight spaces like the pelvis and retromuscular plane where accuracy is challenging even for skilled surgeons. This is a significant advantage over laparoscopic procedures. Surgeons are less likely to develop neck and shoulder pain as they do not have to hold their head in a static position with their shoulders abducted as is the case during conventional minimally invasive surgery [1].
The precision of the robotic system also translates into fewer complications, including hernia recurrence. Studies have shown that r-TAPP is as effective as laparoscopic hernia repair for inguinal hernias, but with better long-term outcomes.
Faster Recovery
When compared to traditional open surgery, Robotic Hernia Surgery is much faster. This is due to the fact that the surgeon doesn’t have to make large incisions to get to the hernia and repair it. This means patients can return to their lives much more quickly after hernia repair surgery, with a less painful recovery.
Hernias are a common condition that can cause pain, discomfort, and even heaviness in the affected area. Typically, hernias develop in the abdominal wall. They can be the result of previous abdominal surgery, such as an incisional hernia, or they may be caused by certain activities like coughing or straining to have a bowel movement.
Traditional surgery involves making large incisions to get to the hernia site and repairing it using mesh. This requires more time off from work and life activities, and can lead to a long recovery with lots of discomfort. It can also lead to increased use of narcotic pain medications, which aren’t ideal for everyone.
Robotic hernia repair, on the other hand, can offer a quicker and more comfortable recovery for patients. During the procedure, most patients are awake and are only numb for the parts of the body where sedation is needed. The surgical robot offers the surgeon a more natural motion with its seven degrees of freedom and 3D vision. It also allows the surgeon to access areas that cannot be reached easily by other methods, such as the pelvis and retromuscular plane.
Most patients can resume their regular daily activities within a few days after robotic hernia surgery, but they should avoid heavy lifting or quick movements until they have been cleared by their doctor. In some cases, patients will be able to go back to their jobs in just a few weeks after the procedure.
The most important thing to remember is that every patient’s experience will be different. Recovery time will depend on how extensive the hernia was and the surgeon’s recommendations. You should always listen to your body and follow the instructions of your doctor, but feel free to ask questions about your recovery process along the way.